© Copyright 2018. All Rights Reserved.
IUI Procedure Tips for Successful Fertility Enhancement
-2023-12-22-6585889f3f1ad.png)
Intrauterine insemination (IUI) involves the meticulous preparation and direct placement of high-quality sperm into the uterus, strategically timed around the woman's ovulation phase. This procedure aims to increase the chances of fertilization by placing sperm closer to the fallopian tubes, where fertilization typically occurs. IUI serves as a recommended fertility treatment for couples facing various challenges, such as mild male factor infertility, unexplained fertility issues, or cervical conditions hindering sperm passage. It offers a controlled and optimized environment for sperm to meet the egg, potentially overcoming specific fertility obstacles and increasing the likelihood of successful conception.
How does IUI work and who needs it?
-2023-12-22-65858976b6f41.png)
1. Understanding intrauterine insemination
An overview of the procedure:
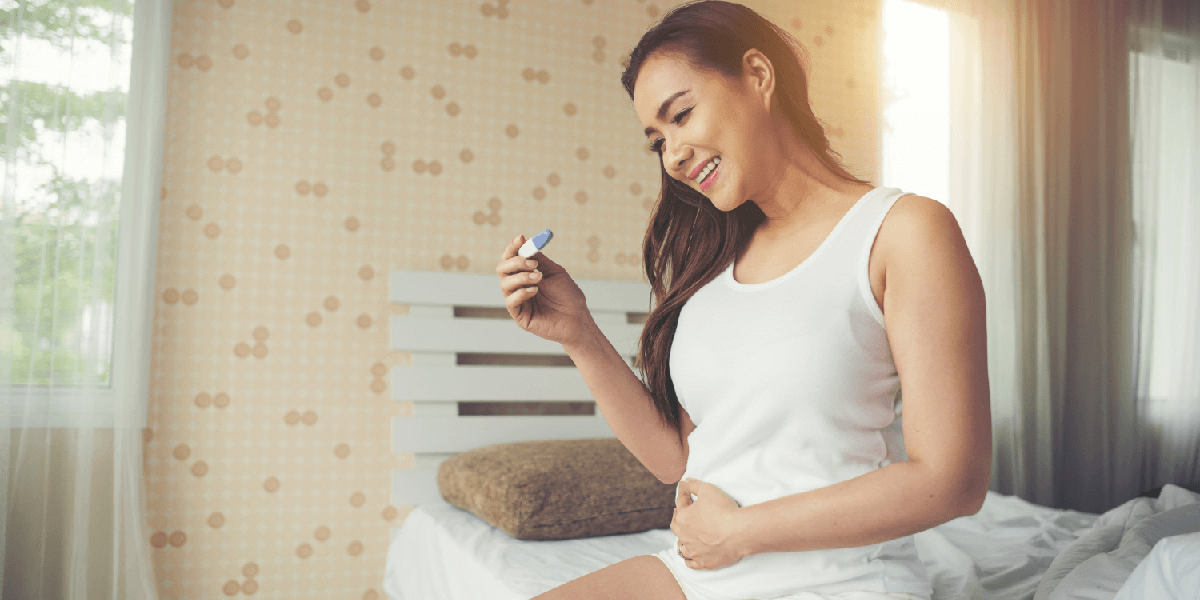
The process of intrauterine insemination (IUI) encompasses several sequential stages, beginning with initial consultations to assess the couple's medical history, fertility concerns, and treatment options. Subsequently, ovarian stimulation is initiated through medications or hormonal therapies aimed at inducing the release of multiple eggs to augment the chances of successful fertilization.
Following this, the critical step of sperm preparation ensues, wherein the sperm sample from the male partner undergoes specialized processing in the laboratory. This process isolates and concentrates the healthiest and most motile sperm, eliminating immotile or abnormal sperm cells.
Once the prepared sperm is ready, the actual insemination occurs. A healthcare professional inserts the prepared sperm directly into the uterus using a thin catheter, typically performed around the time of the woman's ovulation. This strategic timing aims to align the introduction of prepared sperm with the most fertile window, optimizing the chances of sperm meeting the egg for successful fertilization.
Each phase of the IUI process plays a crucial role in enhancing the probability of conception, providing a controlled and assisted approach to assist couples experiencing specific fertility challenges in their journey towards achieving pregnancy.
The objective is:
Consequently, it increases the number of sperm reaching the fallopian tubes and, therefore, the chance of fertilization.
2. Individuals who are candidates for IUI
Male factor infertility encompasses various conditions characterized by compromised sperm parameters, including decreased sperm motility, low sperm count (oligospermia), or mild sperm abnormalities. Reduced sperm motility refers to the inability of sperm to move effectively, hindering their ability to reach and fertilize the egg. Low sperm count indicates a lower-than-normal concentration of sperm in the ejaculate, diminishing the chances of successful fertilization. Additionally, mild sperm abnormalities encompass morphological irregularities in sperm shape or size, potentially impacting their ability to penetrate and fertilize the egg. These factors collectively contribute to male factor infertility, necessitating specialized evaluation and potential interventions to address underlying issues and optimize fertility outcomes for couples undergoing assisted reproductive procedures like IUI.
Symptoms of unexplained infertility:
When a couple encounters infertility without a pinpointed cause, it's referred to as unexplained infertility. Despite comprehensive evaluations and tests, the specific factor hindering conception remains unidentified. This condition can be perplexing and emotionally challenging for couples seeking to conceive. Unexplained infertility prompts fertility specialists to explore various potential factors, such as subtle hormonal imbalances, undetectable abnormalities in egg or sperm quality, or issues related to embryo implantation. Although the precise cause remains elusive, treatments like IUI or assisted reproductive technologies might still be recommended to enhance the chances of conception for couples facing this challenge.
An overview of cervical issues is provided below:
Cervical conditions can pose obstacles to sperm passage within the female reproductive system. These conditions encompass anomalies or disorders affecting the cervix, the lower part of the uterus connecting to the vagina. Certain cervical issues, such as cervical stenosis (narrowing of the cervical canal) or cervical mucus abnormalities, might impede the transit of sperm through the cervix. Cervical stenosis restricts the sperm's entry into the uterus, while irregularities in cervical mucus consistency or production can hinder sperm motility and their journey towards the fallopian tubes for potential fertilization. Addressing these cervical conditions is crucial for couples undergoing fertility treatments like IUI, ensuring a conducive environment for sperm transport and enhancing the prospects of successful conception.
The factors influencing the success of IUI
-2023-12-22-65858e7236df9.png)
1. Choosing the right time
Aligning the timing of intrauterine insemination (IUI) with ovulation is crucial for enhancing procedure success rates. This synchronization involves coordinating the IUI procedure with the release of eggs (ovulation) from the ovaries. By closely monitoring the menstrual cycle and employing techniques like ultrasound scans or blood tests to track hormonal changes, fertility specialists identify the most fertile window for the IUI. This precise timing ensures that prepared sperm is introduced into the uterus when an egg is at its most viable stage, maximizing the chances of successful fertilization. Synchronizing ovulation with the IUI procedure optimizes the conditions for conception, significantly improving the likelihood of achieving pregnancy.
2. The quality of the sperm
The quality of prepared sperm is a pivotal factor influencing successful fertilization during assisted reproductive procedures like intrauterine insemination (IUI). This process involves meticulously selecting and preparing sperm samples to enhance their quality before insemination. High-quality sperm exhibit optimal motility, morphology (shape), and concentration, crucial for traversing the female reproductive tract and fertilizing the egg. Sperm preparation techniques, such as density gradient centrifugation or swim-up methods, aim to isolate the healthiest and most viable sperm, eliminating immotile or abnormal sperm. Ensuring the use of high-quality prepared sperm significantly boosts the chances of successful fertilization and conception, essential considerations in IUI procedures for couples seeking to overcome fertility challenges.
3. A woman's uterine environment
Optimizing a woman's uterine health is crucial for creating an ideal environment that supports successful implantation following intrauterine insemination (IUI). A healthy uterine environment is characterized by various factors, including the absence of structural abnormalities, the thickness and quality of the uterine lining (endometrium), and a receptive environment for embryo implantation. Conditions such as endometrial thickness and texture, hormonal balance, and absence of uterine abnormalities or adhesions are pivotal for successful embryo attachment and subsequent pregnancy. Maintaining a secure uterine environment post-IUI involves assessments, such as ultrasound evaluations, to ensure optimal conditions for implantation, thereby maximizing the chances of achieving a successful pregnancy.
Improving Fertility Through Lifestyle Modifications
-2023-12-22-65859076d6978.png)
1. Taking care of your diet and nutrition
Adopting a nutrient-rich diet significantly contributes to improving fertility outcomes by providing essential nutrients and antioxidants crucial for reproductive health. Essential nutrients like folate, zinc, iron, and vitamins C and E play key roles in supporting healthy ovulation, sperm quality, and overall reproductive function. Antioxidants found in fruits, vegetables, nuts, and seeds combat oxidative stress, which can negatively impact egg and sperm health. Additionally, omega-3 fatty acids found in fish and certain seeds contribute to hormonal balance and reproductive health. Incorporating these nutrient-dense foods into a daily diet not only enhances overall health but also positively influences fertility by addressing nutritional deficiencies and supporting optimal reproductive function.
2. Maintaining a healthy weight through physical activity
Sustaining an optimal body weight while engaging in regular physical activity is essential for supporting fertility and overall reproductive health. Achieving and maintaining a healthy weight range, specific to an individual's body type, contributes to hormonal balance and improves the chances of successful conception. Additionally, regular physical activity, such as moderate exercise routines or activities like brisk walking, jogging, or yoga, positively impacts reproductive function by aiding weight management and reducing stress levels. Striking a balance between a healthy weight and consistent physical activity is pivotal for optimizing fertility outcomes and supporting overall well-being during the journey towards conception.
3. Effective stress management
Implementing stress-reduction techniques plays a pivotal role in mitigating the adverse effects of stress on fertility. Engaging in relaxation practices, such as mindfulness meditation, deep breathing exercises, progressive muscle relaxation, or guided imagery, alleviates stress. Stress reduction is paramount as elevated stress hormones can disrupt hormonal balance, menstrual cycles, and ovulation, thereby impacting fertility. Furthermore, incorporating stress-reducing activities into daily routines supports emotional well-being and positively influences reproductive health, enhancing the chances of successful conception.
The Best Tips for Successful IUIs
1. Be sure to monitor your ovulation closely
Precise ovulation prediction is pivotal for optimizing fertility chances. Ovulation predictor kits, which detect hormonal changes signaling imminent ovulation, offer a user-friendly method for foreseeing fertile windows. Additionally, monitoring basal body temperature (BBT) across menstrual cycles aids in identifying subtle temperature shifts, indicating ovulation occurrence. Combining these methods bolsters accuracy in pinpointing ovulation, empowering individuals to align IUI procedures with peak fertility windows for enhanced conception prospects.
2. Follow Doctor's Recommendations
Compliance with the fertility specialist's guidance is crucial for optimizing IUI success. This entails diligent adherence to prescribed medications, including ovulation-inducing drugs or hormone therapies, ensuring they're administered as directed. Moreover, meticulous observance of the suggested timing for the IUI procedure, aligned with the individual's ovulation cycle, significantly heightens the likelihood of successful conception. Consistent and precise adherence to these instructions, in tandem with professional recommendations, plays a pivotal role in enhancing the effectiveness of IUI treatments for prospective parents.
3. Ensure Sperm Quality
A holistic approach to fostering optimal sperm quality involves embracing a healthy lifestyle. This encompasses dietary modifications rich in antioxidants, vitamins, and minerals known to bolster sperm health. Additionally, regular physical exercise aids in weight management, potentially improving sperm parameters. Steering clear of harmful habits like smoking and excessive alcohol consumption is paramount, as these can detrimentally impact sperm quality. Prioritizing adequate sleep, managing stress levels, and minimizing exposure to environmental toxins further contribute to fostering an environment conducive to enhanced sperm quality, consequently augmenting the prospects of successful insemination.
4. Minimize Stress
Incorporating stress-reduction practices plays a pivotal role in fostering a conducive environment for successful fertility journeys. Activities such as yoga, meditation, or mindfulness exercises offer profound benefits by alleviating stress levels and promoting overall well-being. Moreover, engaging in hobbies or pursuits that evoke relaxation and joy serves as a therapeutic outlet, alleviating the emotional burden often associated with fertility challenges. By integrating these relaxation techniques into daily routines, individuals can effectively manage stress, enhancing their mental and emotional state throughout the fertility journey, positively influencing the chances of a successful outcome.
Medical Interventions and Support
1. Ovulation Induction
-2023-12-22-658591657755f.png)
Utilizing hormonal treatments aims to induce and regulate ovulation, a pivotal step for optimal timing in the IUI process. These medications, such as gonadotropins or clomiphene citrate, work to stimulate follicular development and trigger ovulation, aligning the procedure with the most fertile window. Carefully monitored hormonal therapies, administered under the guidance of fertility specialists, aim to enhance the chances of successful conception by precisely timing the IUI procedure with ovulation, optimizing the conditions for fertilization and increasing the prospects of achieving pregnancy.
2. Sperm Enhancement
Refinement of sperm quality involves employing specialized techniques for sperm preparation. These processes, including sperm washing and density gradient centrifugation, aim to isolate high-quality sperm from seminal fluid. Sperm washing entails separating motile and morphologically normal sperm from other components, enhancing the concentration of viable sperm for IUI. Similarly, density gradient centrifugation utilizes density gradients to isolate motile and genetically superior sperm, optimizing the sample for insemination. These meticulous sperm preparation methods, conducted in clinical settings under stringent protocols, play a pivotal role in augmenting the chances of successful fertilization during IUI procedures.
3. Uterine Cavity Assessment
Employing diagnostic techniques is crucial in evaluating and optimizing the uterine environment for enhanced IUI success. Procedures like hysterosalpingography (HSG) or hysteroscopy enable a comprehensive assessment of the uterus, identifying potential abnormalities or obstructions that may impede the success of IUI. HSG involves a contrast dye to visualize the uterine cavity and fallopian tubes, offering insights into any structural issues. Hysteroscopy, a minimally invasive procedure, utilizes a thin, flexible instrument equipped with a camera to directly inspect the uterine cavity, detecting and addressing any abnormalities that could hinder successful insemination. By meticulously evaluating and rectifying uterine conditions, these diagnostic techniques play a pivotal role in optimizing the uterine environment, thereby enhancing the chances of successful IUI outcomes.
Conclusion
-2023-12-22-658592d980c32.png)
IUI serves as a beneficial fertility treatment for couples facing specific challenges in conceiving. By integrating lifestyle modifications, medical interventions, and procedural insights, individuals can significantly enhance their chances of successful conception through IUI. Seeking professional guidance from fertility specialists plays a vital role in optimizing the success of IUI treatments.
This updated guide incorporates an expanded section dedicated to providing detailed tips for enhancing IUI success. It emphasizes the importance of closely monitoring ovulation, following the doctor's recommendations, ensuring sperm quality, and minimizing stress to maximize the likelihood of a successful IUI procedure.
Recent Post
-
The Connection Between HCG Hormone and Pregnancy: Explained in detail
-
Conquering Asthenozoospermia: Strategies for Male Fertility Success
-
Embracing Sensuality with Vaginismus: Strategies and Support
-

Understanding Endometriosis: Symptoms, Causes & Management | Guide
-
Decoding Erectile Dysfunction: Insights, Remedies, and Resource & care